Cuba is undergoing a transformation in its health services and the guidelines governing said services. The transformation focuses on the analysis of the most persistent challenges in the country, and the implementation of economic and social policies to address them.Several changes have been implemented occurred and are looking at this perspective, and within them, new transformations in the National Health System (NHS).
In the mid-1990s, the Ministry of Public Health began a new moment of transformation of the sector, with the objective of defining the main strategic lines and programs, which would allow a process of consolidation and modernization of the system to be developed. new methods and work styles. Since then it has been argued that spending on health increased, and consequently limited other activities and budgeted branches. 2
At the beginning of the last decade, numerous social programs were implemented, inscribed in what was called “Battle of Ideas”, within which, actions were designed for the recovery and improvement of the system, integrated in the so-called “Revolution in the sector Health”. At the end of 2010, a process of “Reorganization, concentration and regionalization of health services” was announced, which had among its antecedents the speech given in December 2009 by the President of the Council of State of Cuba and in which it stated that “without affecting the quality of health, which is provided free of charge to all citizens, and even improving it, it is possible to significantly reduce expenditure.” 3
Taking into account these premises, a contextualized approach of the recent evolution and the current situation of the health services in the country will be tried, by means of the formulation of some questions: How is integrated the revolution of the sector initiated in the last decade, to the current transformations? What can be the main obstacles in achieving the new objectives?
DETERIORATION OF SERVICES AND REVOLUTION IN THE HEALTH SECTOR
The primary effects of the deep economic crisis that the country faced in the early 1990s, and their side effects, resulted in the infrastructural deterioration of facilities, serious shortages of material resources, deficiencies in professional performance, lack of managerial training for the driving the health system at the unit level, coupled with increased demands for hospital care, and increasing population dissatisfaction, including emergency care. 1.4 The results of the national survey on user satisfaction with health-care services of the Ministry of Public Health in 1990 showed no favorable situation: approximately 70 per cent of the population were moderately satisfied and 10, 6% dissatisfied, a situation that worsened in subsequent years.
In this regard Suárez, 1997 states:
… The impact of the crisis on health services presents challenges difficult to solve in a country with a universal and free health system, a population accustomed to making extensive use of services, including those of advanced technology and a reality in which access to external credits on the one hand, and markets for medicines, supplies and medical equipment on the other, is made difficult by the effects of the blockade, which increases and limits its acquisition … 5
Since the mid-1990s, the Ministry of Public Health started studies to diagnose the situation of the NHS and to draw up strategies for the recovery of the sector, focused on improving the quality of services, efficiency, effectiveness, and maintain equity. 1
Priority lines were defined as the reorientation of the health system towards primary care, the revitalization of hospital care, the reanimation of the work of state-of-the-art technology programs and research institutes, the development of the Medicines and Natural Medicine Program and Traditional, as well as priority attention to objectives such as emergency, stomatological and optical services. Programs of maternal and child care, chronic noncommunicable diseases, communicable diseases and the elderly were considered to be of the highest priority. The so-called “Health Revolution Programs” were structured at the beginning of the last decade, with the objectives of perfecting the system in general and primary health care in particular and resumed in the processes of reforms already initiated. They reaffirmed the need for changes in the organizational structure of the system, especially in ambulatory care, the organization of services and health programs. 6
One of the actions in the concretion of such efforts was the organization of the “Program for the Reconstruction and Modernization of the Polyclinics”, which proposed the approach of services to the population, the adaptation of these services to the health situation of each training and continuous improvement of human resources, as well as the improvement and introduction of new technologies. 5
The polyclinics were repaired and their services were expanded through the transfer of technology from the secondary and tertiary levels (general and specialized hospitals) to the first level of attention, to an unprecedented extent. 7
The polyclinics were endowed with an average of 20 services, which exceeded 30 in some of them, such as rehabilitation, radiology, ultrasound, optometry, endoscopy, thrombolysis, emergency services, traumatology, clinical laboratory, family planning, dental emergencies, maternal care immunization, care for diabetics and the elderly, as well as consultations in the specialties of internal medicine, pediatrics, obstetrics and gynecology, dermatology, psychiatry and cardiology.The repair and renovation or introduction of technological equipment also benefited the secondary services included in the other “Hospital Reconstruction and Modernization Program.”
In parallel, there was a gradual closure of doctor’s and family nurse’s offices, the population attended in several clinics in one, and although the coverage of care was maintained in 100%, multiplied the population to attend , with the consequent recharging of the work of the doctors and nurses that seriously affected the attention previously given, and especially the perception about it.There was no change in the priority accorded to some programs, such as maternal and child care (PAMI), and weakened promotional activities and field work, functions intrinsic to this program (scheduled visits of the doctor and nurse to housing where the population resided vulnerable within care programs).
The reduction of clinics and the compaction of the services provided by the doctor and the family nurse has been associated with the massive departure of physicians to perform collaborative missions in several countries, while other opinions emphasize the serious organizational problems faced by the Medical and Family Nurse Program (PMEF), and not the lack of doctors at this level of care. 8.9 This reduction was included, the continued infrastructural deterioration of clinics, and the lack of work materials.
Consequently, the population’s dissatisfactions, associated with the instability of the services, the waiting time for attention, the absence of the doctor for fulfilling other administrative functions or new teaching tasks, as part of the “adaptation” to a new doctor in the territory.This situation is complicated by the total or partial closure of hospital institutions and therefore of more complex services, in the context of the reequipment of hospitals or polyclinics in repair.The perception was even more negative because of the previous care reference, especially when the clinic should be the gateway to the more complex and specialized care system, many of which would now be available in polyclinics.
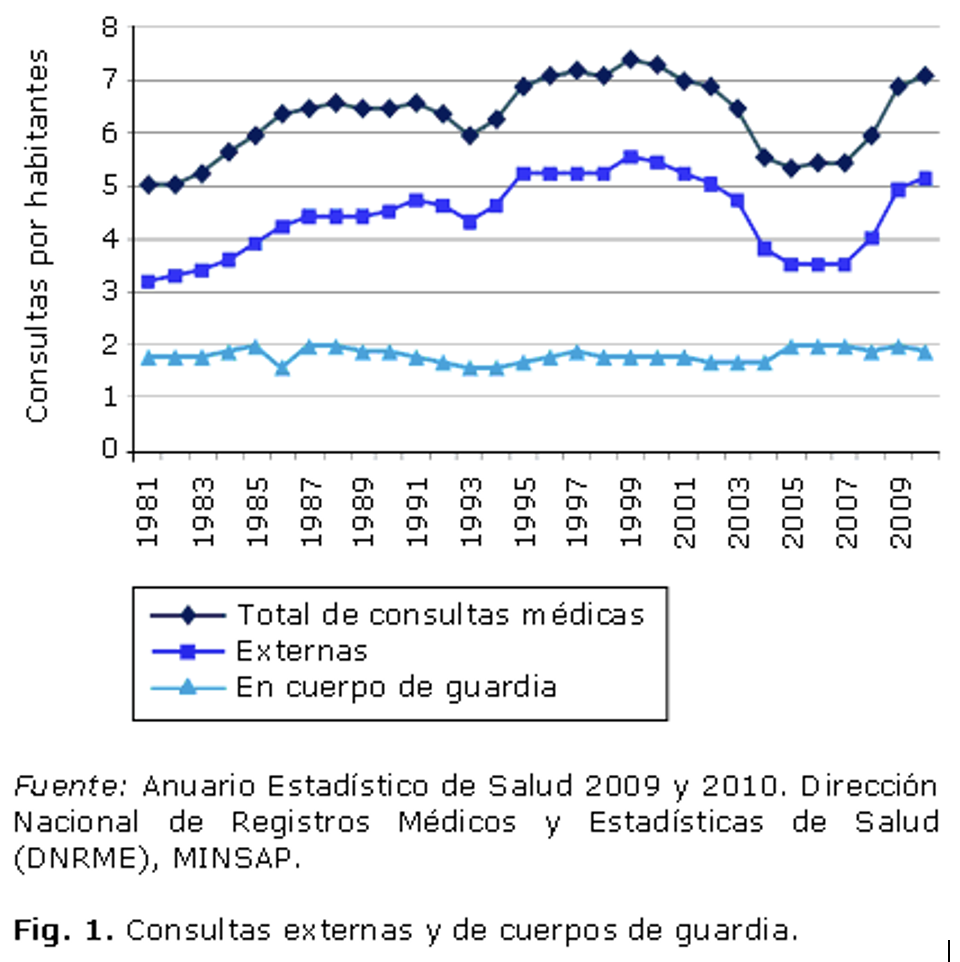
The reduction observed in the number of total medical consultations at the beginning of the last decade, came to two consultations less per inhabitant between 2002 and 2006, a more remarkable decline even than the one produced in the decade of 90. It is worth commenting that the decline was more acute than that experienced in 1993, a year of increase in the incidence of some nosological entities, which demanded the intensification of active researches that may have influenced the reduction of consultations ( Fig .
Taking into account this situation, as part of the reorganization of primary care, from 2008, when the tax population to a clinic was up to 2,500 people, a typology (I, II and III) based on hours of operation, and human resources allocation based on factors of location and access to other health institutions.Type I worked eight hours a day, half a day on Saturdays and one day a week until late at night, with a multidisciplinary team that served an average of between 2,500 and 3,000 people.Type II with nurses eight hours, guaranteeing the doctor-oriented tasks to the population and type III, with doctor and nurse 24 hours a day, located in the most remote places.
The recovery of the number of external consultations as of 2008 suggests the positive influence of such reorganization.
Coinciding with these inflections, the surgical activities seriously affected since the 1990s, maintained a tendency to decrease in 2006 to less 58,000 surgeries in relation to the previous year, a fact that suggests the loss of the system’s capabilities to satisfy the demand for this service, within the framework of repair and modernization programs under way in the institutions, without overlooking the resource limitations in these medical practices.
Some indicators of facilities for the care of vulnerable groups, such as pregnant women and the elderly, varied the availability of their services, where a possible reduction in demand may also have occurred. Those housed in nursing homes in the internal regime remained stable during the 1990s and early 2000s, to experience a slight reduction maintained from 2003 on the order of just under 300 elderly beneficiaries in 2004 ( Fig 2 ).On the other hand, those of the semi-formal regime experienced an intense growth in the same period.
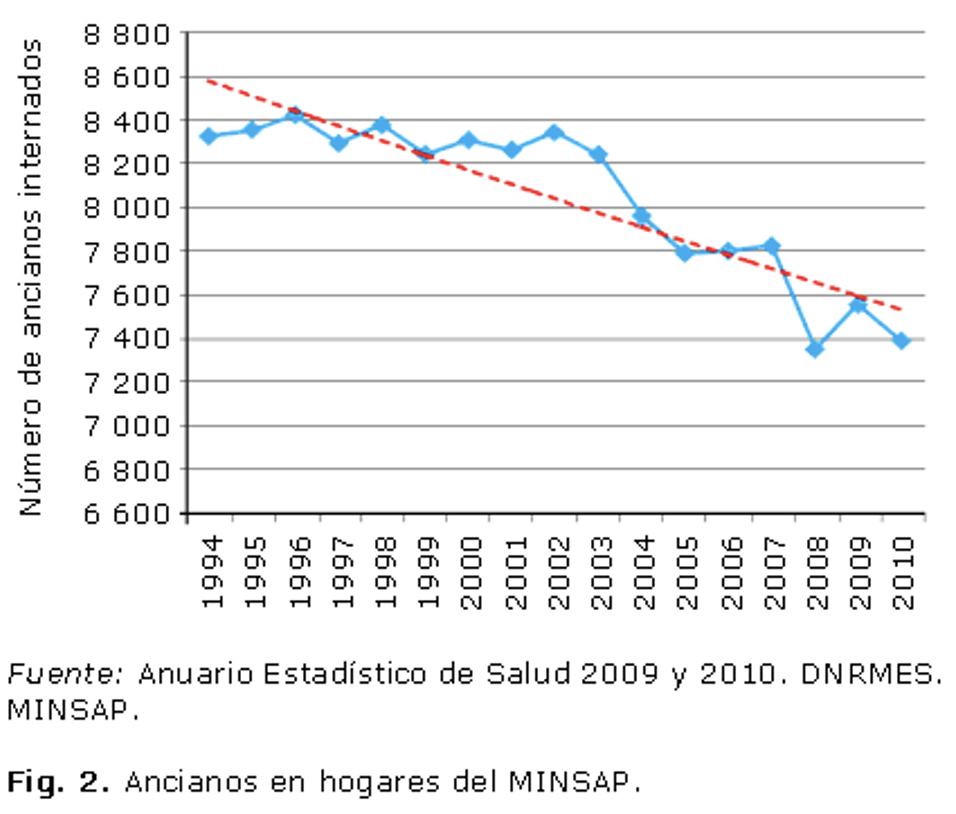 Other resources and services for these population groups continued to be provided in institutions such as grandparents’ homes, comprehensive care for the elderly and local variants of care, which included social assistance in the residence of adults in conditions of social vulnerability.
Other resources and services for these population groups continued to be provided in institutions such as grandparents’ homes, comprehensive care for the elderly and local variants of care, which included social assistance in the residence of adults in conditions of social vulnerability.
Maternal households are organized by the need to bring pregnant women to hospital, in addition to prenatal care, nutrition is taken care of and health education is given priority in the promotion of breastfeeding and child care. These institutions increased the income of pregnant women, with a decrease since 2002, which, as in previous descriptions, reached its lowest figures in 2006, with just under 70,000 women hospitalized, to experience an increase thereafter exponential that reached its maximum value in 2010, for an indicator of 50.8 admitted to maternal homes per 100 live births (including pregnant women in homes with a pre-natal regime). ( Fig. 3 ).
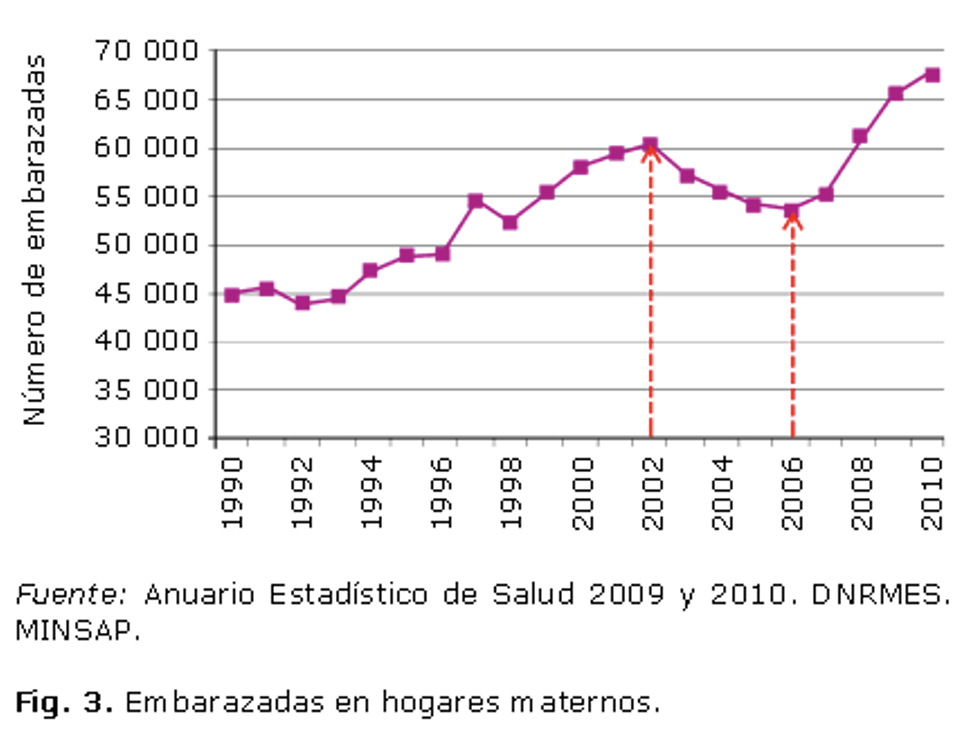 This may be associated with different factors, such as the adoption of an alternative in the form of a semi-permanent regime, the increase in the number of births in the last two years of the period under review, and the priority that PAMI proven effectiveness.
This may be associated with different factors, such as the adoption of an alternative in the form of a semi-permanent regime, the increase in the number of births in the last two years of the period under review, and the priority that PAMI proven effectiveness.
The priority accorded to the health sector since 1959 saw a notable increase in the implementation of the budget and a particular rise in the first decade of this century, more intense since 2006, consistent with the consolidation of the aforementioned programs of the revolution , to arrive in 2009, 10 to its highest figure of 440.30 pesos per inhabitant ( Fig. 4 ).
 The increase observed in the number of health workers in the 80’s due to the implementation of the PMEF, is from 2002 and especially in 2006, much more intense, explained essentially by the incorporation of workers linked to the new or extended services in the polyclinics, and because a continuous teaching process was conceived of this professional, so that at the end of the first year of study, they became workers, without discounting the discreet salary increase applied in the middle of the 2005.
The increase observed in the number of health workers in the 80’s due to the implementation of the PMEF, is from 2002 and especially in 2006, much more intense, explained essentially by the incorporation of workers linked to the new or extended services in the polyclinics, and because a continuous teaching process was conceived of this professional, so that at the end of the first year of study, they became workers, without discounting the discreet salary increase applied in the middle of the 2005.
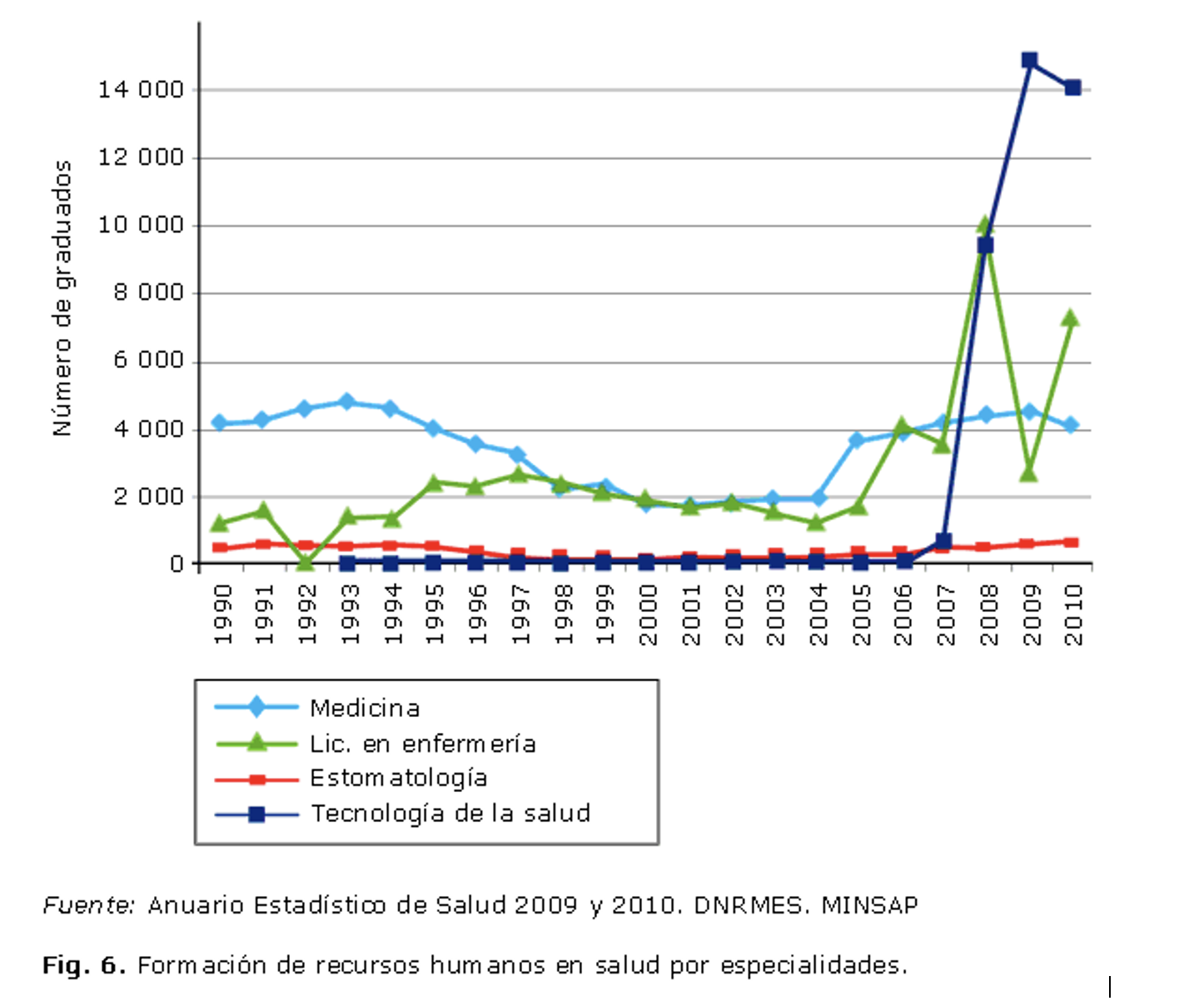
Thus, the formation of human resources in health with a remarkable growth in the decade of the 80, experienced a reduction from the end of the decade of the 90, to assume a remarkable increase from 2006 and reached in 2010 the figure of 26 600 graduates of the higher education of the different specialties. This fact is basically explained by the number of professionals trained in health technology, 10 who, according to the applied teaching scheme, were incorporated as workers and paid wages at the end of the first year of study ( Figs 5 and 6 ) .
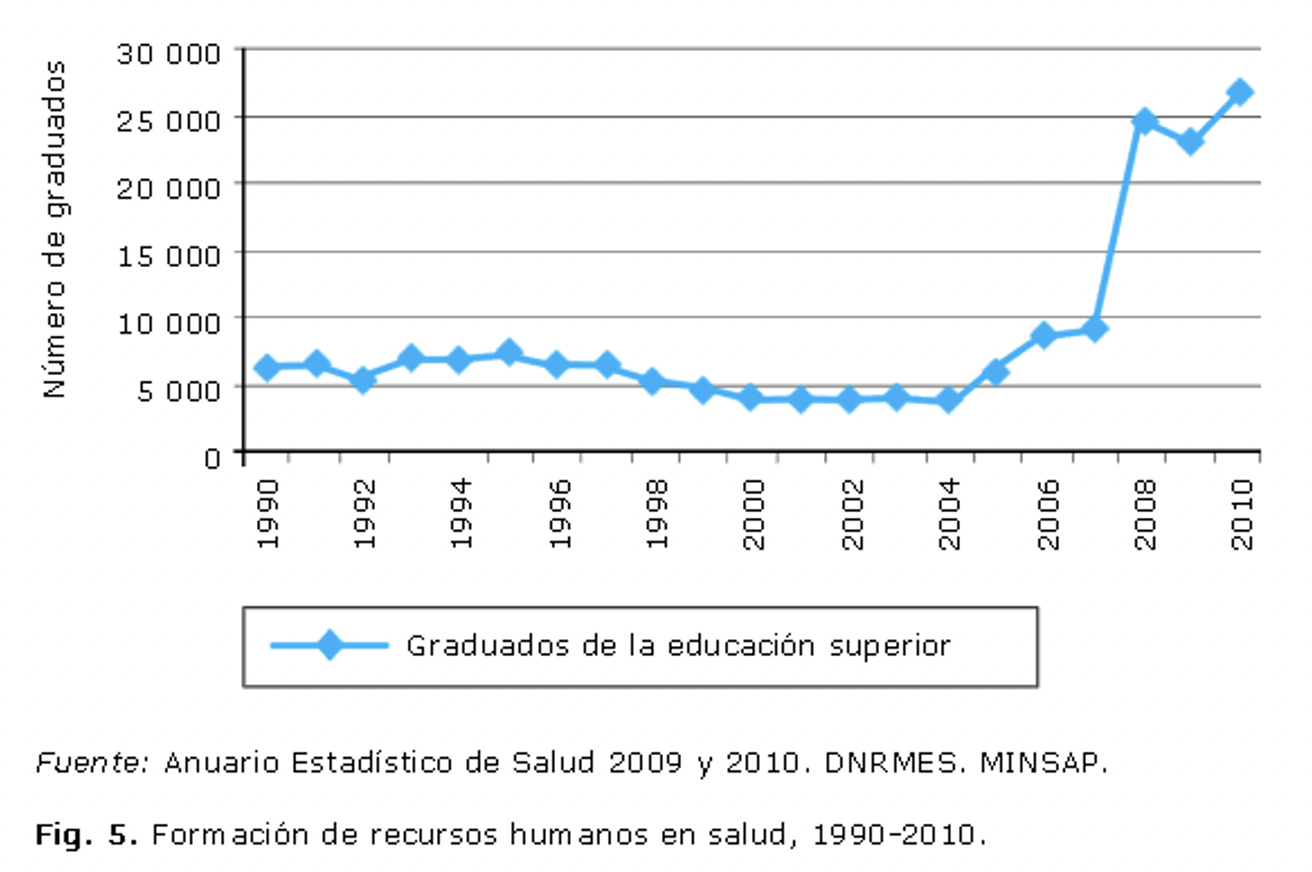
The structure of health workers by occupation in 2009 shows that the highest indicators were obtained in the abovementioned occupations with 119 average technicians per 10 000 inhabitants and 86.5 in nursing personnel per 10 000 inhabitants. In that same year there were 66.6 doctors per 10 000 inhabitants, and 10.3 stomatologists per 10 000 inhabitants. At the end of 2009, 74,880 physicians were active, of which 73% were specialized. The largest number of doctors corresponded to those trained in general general medicine (45% of the total), with 75% of them specialists, followed by those dedicated to health organization and administration (approximately 20% of the total) with only 5% of specialists. Other of the most represented physicians were dedicated to internal medicine, obstetrics, and pediatrics. 10
The movement of service indicators at the beginning of the first decade of 2000, coinciding with the beginning of the implementation of the Programs of the Revolution in the sector and the growth in the total number of workers, per capita expenditure, and the training of workers in some specialties, as part of the steady increase in the number of doctors per inhabitant, which by 2010 reached a figure of 68.1 doctors per 10 000 inhabitants. eleven
The inflections observed, the decline in the early 2000s and the recovery since 2006, suggest the influence of the programs under way, with different expressions in the territories, which move between the reduction of the supply of services, or the opposite of demand, according to the stage of reconstruction and modernization of health institutions.
As has been noted in a number of publications, internationally relevant health indicators, such as infant mortality, under-five mortality, infectious disease and other diseases, have generally not deteriorated or even improved, which is not only explained for the priority that the respective programs of care have maintained since the creation of the SNS, as well as by advances, although in a differentiated way according to groups in social spaces, in dimensions of living conditions in the last decade.
On the other hand, the positive impact of the reconstruction and modernization programs of polyclinics and the increase of services in these can be seen in the proportional displacement of the consultations towards them. In 2010, about 90% of total outpatient consultations and 65% of all emergency consultations were performed in the polyclinic. eleven
A final and delicate aspect, it participates in the network of components and processes in which the programs for the recovery of the quality of the health services in the country evolved. These components are more difficult to measure, conformed in the subjective-objective duality of these processes that cause side effects such as the demotivation towards the work and the perception of inequality of the workers of the sector. Although the need to deepen the spiritual motivation of workers to achieve full compliance with the social order of public health is absolutely certain, 5 it is also necessary to go deeper into the analysis of the material living and working conditions of professionals and in general of workers in the sector.
It is well known that the majority of Cuban doctors who have not performed internationalist missions, or benefit from some other sources of supplementary income, even from non-work, such as family allowances and remittances, are generally citizens who experience similar economic, to other workers in the country (professional or not), which is reflected in the acknowledged gap between supply and demand, or demand without supply, and many other limitations in meeting basic needs, traditional or new satisfiers of old needs .These situations are not exclusive to Cuba, although they are rare in other countries, where professions of high social representation such as doctors, nursing, rehabilitation specialists, among others, are often distinguished as a stratum in income advantages.
CURRENT TRANSFORMATIONS IN THE NATIONAL HEALTH SYSTEM. DISTRIBUTION AND EQUITY IN FOCUS
The Ministry of Public Health recently produced a document on the transformations of the NHS, which we will use to analyze the current proposals. 12
The document considers that the transformations will allow:
… the most efficient and rational use of the large and expensive resources we have, especially the technological ones, as well as their permanent availability, which will guarantee the sustainability of health services.
Although the initial motive is undoubtedly economic, it is evident that in these transformations, other elements are considered, and as the above document states, the transformations pretend to assume the “urgent need to reach higher levels of efficiency and quality.” 12 In a coherent way, the first of the guidelines of the health sector contained in the guidelines of the country’s economic and social policy, approved recently, proposes “to enhance the quality of services and the efficient use of resources, subsequent expenditure “.According to official figures during the decade of 2000, the execution of the budget did not decrease and for 2010 a reduction of little more than 10 million pesos is observed.
It is explicitly stated that the reorganization of the management structures must respond to the needs of the health situation in each territory, with the personnel strictly necessary and with the qualification and experience that allows to achieve efficiency in the work.Along with the reduction in the number of workers expected, it is considered that those who lead, must have been transited by the system, before occupying a management position at any of the levels of care, and possess the necessary qualification and experience.Also associated with the qualification, the need for doctors to apply the clinical and epidemiological method, as the main guarantee of the quality of health services, is consistent with the loss of attention to these methods, and the priority given by the physicians and population to diagnostic technologies.
The regionalization of services is considered the way to maintain the achievements in the technical and material order of the health sector, given the economic situation facing the country, and is based on a territorial redistribution of services, exemplified in :
… a team provides its service in a health area, in a municipality or in the provincial head, in correspondence with the existing activity level and there the population comes to receive it, which also allows the specialists and technicians of greater preparation provide the service, ensuring greater quality. 12
Thus, the analysis and proposals for the redistribution of services, especially in primary care, most of which were implemented in recent years within the framework of the health revolution, such as rehabilitation, endoscopy, regulation menstrual, imaging, minor and emergency surgery, among others, and it is advised that in cases where underutilization is demonstrated, be regionalized, to expand the number of beneficiaries and the number of settlements, or municipalities that make up the area that taxes to the services in question.
The regionalization processes represent one of the main readjustments to the criterion used in the revolution of the sector deployed in the last decade, – to increase the population to the services, before the necessity of a distribution whose rationality assures the maintenance of some of them.While it is true that this is a way to ensure the highest quality, the accessibility aspect is a factor that can restrict the expected achievements of this regionalization, in terms of satisfaction and others.
In relation to the distribution of polyclinics, it is proposed to re-analyze the level of activity and the human resources needed in those that serve less than 5 thousand inhabitants, and in the case of verifying the underutilization of resources or services, these will be converted into medical offices, redefining their functions according to the population universe to be served.It is this other delicate criterion that can put at risk the distributive equity.
The hospitals also consider the evaluation of their services and the occupational index, to readjust the material and human resources. In cases where their permanence is not justified, they will be compacted or regionalized. In fact some results of the regionalization in provinces such as Villa Clara already consider the reduction of hospitals and their conversion to other functions, such as nursing homes, or polyclinics with beds. 13
An important activity of reorganization is that referred to 24% of the municipalities of the country, where there was only one health area, ie a single polyclinic, and also a Municipal Health Department, which are now merged, so that the polyclinic assumes the management and administration of the system, eliminated duplication of functions.The health area is defined as the territorial space, with defined geographical limits, in which a population that receives integral health care through a polyclinic resides.
Within the framework of transformations, in the doctor’s offices and the family nurse, the population to be served is redefined, the number of those who will provide stable services, and the human resources needed in them, with a population of up to a maximum of 1,500 inhabitants in consultations and field work.This means that from an average of 120 to 160 families to be served until 2004, and the increase that occurred in the middle of this decade, which reached more than 600 families, will produce a reduction that on average represents the attention of 300 to 400 families per office.
It is striking that the number of families or individuals who belong to the tax area to a clinic, or a polyclinic, although with certainty considered, does not have, we know, definition of extension, distance or time to access from the population settlements to services, components that become decisive in some contexts, particularly in concentrated or dispersed rural or mountain settlements, or in those that have had negative impacts on the most recent economic processes, such as the closure of sugar mills and others, where transport services are seriously affected.
On the other hand, the revitalization of family medicine with the reopening of clinics has been reported by different media, with previous distributions resuming, with the consequent recovery of some of the functions that had been seriously affected. This is undoubtedly an important way to improve the availability of primary care services and, potentially, the satisfaction of the population with services in the community. 14,15 In Havana, a similar process is known, which in some cases takes as a variant the division of the population to be attended by the doctor and the family nurse in two offices operating within the same facility.
Another of the transformations refers to the analysis of the rationality of ambulance services, through changes in the organization of the places where they are located (bases).These measures, which immediately reduce expenses and increase controls, require careful monitoring of their effectiveness, since they are usually urgent, and the delay in receiving the service is decisive for the solution of the health problem in question .
The reorganization of care services for pregnant women in maternal homes is based on the occupancy rate (pregnant women per maternal home), the distance to polyclinics with beds, and the rapid access to the corresponding gynecological and obstetric hospital, which is why numerical reduction of these and with it, their organizational structures.
Some results of the transformations in progress show that in maternal homes with a capacity of only three or five beds, there are an average of 20 workers, and some of these households are close to care units that can guarantee care for pregnant women, 16 compaction of these services has already caused their reduction, as in the case of the province of Villa Clara. 13
An observation of particular interest is the reanalysis of study offers in some specialties of the sector, such as health technologies.It is recognized that one of the causes of “excessive number of workers” is associated with an increase in the training of human resources in some specialties, especially those trained in health technology careers, which is explained by having taken into account the needs of the territories, for the offer of enrollments in the corresponding institutions.On the other hand, in some territories, there are shortages of services of some specialties, basically medical, that must be solved.
The transformations in progress have an integrated conception, and this has been pointed at the world level as key to the success of reforms in health systems, given that in order to expand the vision on these systems, it is necessary to think, in addition to its components, such as financing, institutions and technologies, think about their interrelationships. 17
In the new transformations of health services in the country, the territorial dimension has special significance and is directly associated with the multiple objective and subjective, instrumental in the implementation and consolidation factors. Documents and other information about the current process of “reorganization, concentration and regionalization of health services” in the country, argue that territorial information is taken into account.
This process closely linked to the territory, the population distribution and characteristics of the settlements, there must be further defined a new figure tributary population to the institutions of primary level, distances that would these services each settlement or neighborhood and mobility conditions to services relocated, or real accessibility, regardless of distance, a factor that can be decisive, given the limitations of the more severe public transportation among some settlements in the country, and prices of private transport which certainly they are not accessible to the income of many families.
In the theory of geography of services, it is considered that the distribution or redistribution of any of them, always leaves the lead on the population of a territory, and at a disadvantage relative to the other. Optimal distributions, in the case of health services, whose budget is assumed by the Cuban State absolutely, are required at this historic moment to balance economic rationality, with equity, which is considered synonymous with equality strict sensus by the Cuban population.
In the revolution of the beginning of the last decade sector they may have been decisive criteria such as differences in population territorial context, location in relation to other services, accessibility of the population to services, health status, problems and needs, among others, yet they were structured without the pressure of budgetary restrictions, or at least without the priority the economic rationality imposed right now.
Added to this is integrated, that as a result of invoking a distorted equity in the country have implemented policies, standards, and strategies for action in many sectors with an egalitarian territorial distribution. In the case of health, the distribution of resources and services, especially those related to modern technology sector is much more difficult to define parameters of equitable distribution, without some resignations, the strong humanitarian component and the political will that he fed them prior distributions. It is not now to bring the population to services, but that the population transfer services in places where they will be assigned.
The current complexity is crossed not only by the geographical distribution of the population within municipalities, and the different economic and social contexts of these. Although not intended to thwart acquired rights “remoteness” which will be on some services, could create new dissatisfactions.
Raise awareness of the risks of using high-tech equipment, self-medication, or the benefits of natural and traditional medicine aspects are also considered in the policy guidelines of the sector, is not achieved quickly, they are required educational activities and individual favorable, experienced or credible or family experiences in these aspects. The entries in various media that targets a habit acquired correction, communicate this information to the population may have the opposite effect than expected. That is why, there is not always a direct relationship between increased services and quality, or vice versa, or between the quality expected and perceived by the population, especially when still it hurts the benchmark high quality primary health care, built for more than two decades.
territorial differences should be expected in the progress of transformations, or the quality of care will be the same in all territories, and with the same services in both territories will be equal satisfaction. Clearly, in the capital, expectations, especially high-tech services, are higher if compared with those in mountainous areas of eastern Cuba. With health administration, other sciences such as economics, geography, sociology, psychology, anthropology and statistics, will have much to contribute in the complex approach to issues of distribution and equity, both theoretical order as practical, not only in the sector in question, but in the rest of the sectors that make up the public health.
FINAL THOUGHTS
The proposed policy guidelines of the health sector in January and reorganization processes, compaction and regionalization of health services under way, indicate that we walk by further changes in the Cuban SNS, which aim to reduce costs in the sector in the short term, a fact already noted in recent years, with considerable savings in various activities.
Raising the quality of services included in the guidelines of health policy, and satisfaction of the population, will not have such immediate results, and somehow will be conditioned to the improvement of material living conditions and spiritual the two human components of the system, which always participate in a dual role: service providers-citizens and noncitizens patients.
Hard work of attention to these components, and an intense articulation of them, with complex relationships established between financing, organization and management, will be key to progress towards recovery services, improved care and permanence of care achievements. The health is not only a specific sector of public administration, but a social priority objective; in the case of Cuba there is ample evidence of progress towards this goal, which can not be seen as figures achieved in relevant indicators globally, but as a result of the implementation of a strategy and deployment of essential public health principles. 18
In 2006, Rojas Ochoa, one of the most important sanitaria’s the country, placed in an interview published in the magazine Temas, the major stages of the model health care in Cuba:
… an initial, not yet well characterized integral policlínico; the Community Polyclinic; and family medicine that seems to be coming to what happened to the others, at a time that does not satisfy all demands. The model is running out, and we do not know how to emerge the new. 19
At the request of the journalist, advances some hypotheses about what might come:
I aspire, I do not know if it’s going to come or not to something closely linked to the formation of the attending physician more to the social dynamics of health and disease. More health promotion … greater attention to the social problems that have to do with human health … it is necessary that the new model not give him so much cult of high technology, let us lay us a bit in the old procedures, as effective as the clinic. 19
More recently, in a totally proactive behavior, Rojas Ochoa, writes ten , “necessary corrections”, 20 coincide almost entirely with SNS transformation measures that months later proposed by the Ministry of Public Health.
“Necessary corrections” of Rojas Ochoa, included in the document under the title “necessary transformations of the Public Health” 12 mentioned, differentiated fundamentally, the importance of this public health professionals gives the need for stimulation those who perform their daily tasks heroically, both in missions abroad and in Cuba , and marked priority to the training and development of human resources in health.
It stands out in this proposal, priority to the social problems of the population and stimulating sector workers, among others.
Strengthening health promotion also included in the policy guidelines of the sector, and the set of actions associated with it requires perhaps more than in other sectors, the close and harmonious relationship between -prestadores and beneficiaries. It is well known that sector policies are not sufficient to protect, improve or maintain the health of the population and require the integration of many sectoral policies, and the well known and yet to perfect intersectoriality key to improving health Social.
Humanist essence of the Cuban social system will not change, as it has done in other difficult circumstances, and with as many goals especially updating the economic model, certainly will seek to preserve and improve the health of the population. Advances in nutrition, housing and proper hygiene, stress reduction, satisfaction with the occupation, and many other components that determine the social construction of health, will be achieved to the extent that progress in the implementation of many of the country’s political and economic guidelines, not only those related to the health sector.
Held free and universal coverage, the NHS is facing in the current circumstances to reconcile economic rationality and quality, but in parallel need to rework the concept of equitable distribution of resources and services, and encourage the population to rebuild their perceptions and reference on health care.
