Breast Cancer Treatment Program
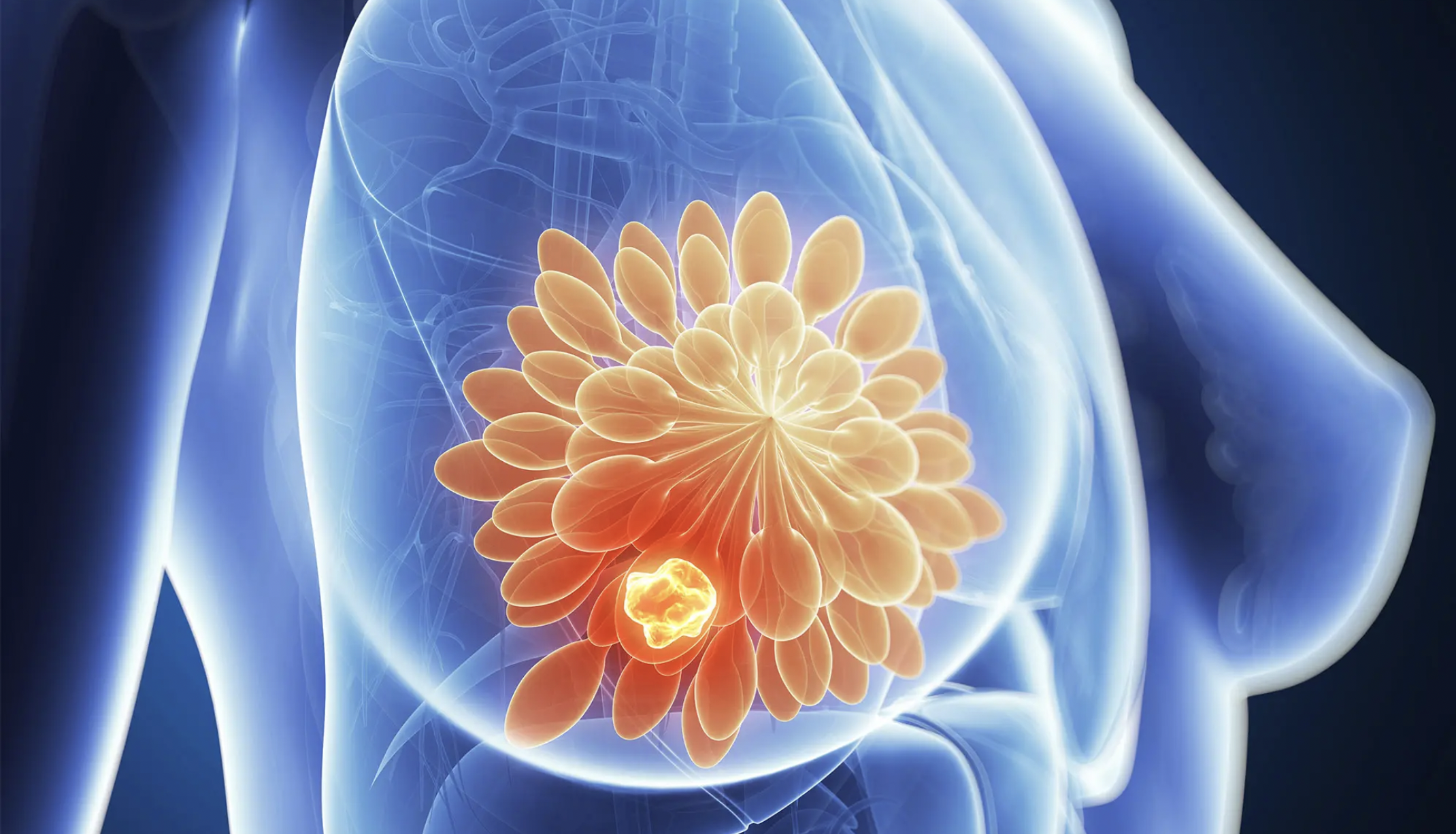
Breast cancer is the most frequently diagnosed malignancy in women globally and remains a leading contributor to cancer-related mortality. Although it predominantly affects women, male breast cancer, while rare, does occur and accounts for approximately 1% of all breast cancer cases. In both sexes, the disease arises from the epithelial cells of breast tissue, most often within the ductal or lobular structures, though in some cases it can develop in the connective or stromal tissues that support the glandular architecture. The biological behavior of breast cancer can vary widely—from slow-growing, hormone-sensitive tumours to aggressive subtypes with early metastatic potential.
Despite significant progress in screening and treatment strategies, breast cancer continues to pose a global health challenge, particularly in regions with limited access to timely diagnosis and comprehensive care. The disease’s potential to affect regional lymph nodes, chest wall structures, and distant organs underlines the importance of a multidisciplinary approach to management. Advances in molecular profiling, imaging, and minimally invasive surgical techniques have improved clinical outcomes, but the key to long-term survival lies in early detection, precise staging, and individualized treatment planning. As breast cancer can present differently across sexes, age groups, and biological subtypes, a tailored and patient-centered approach remains essential in achieving optimal results.
Why Cuba
Breast cancer treatment in Cuba is delivered through comprehensive, multidisciplinary oncology programs tailored to the precise diagnosis, management, and long-term care of both female and male patients. These programs integrate the expertise of Cuban medical oncologists, surgical oncologists, radiologists, pathologists, and reconstructive surgeons—supported by the country’s well-established public health system and emphasis on preventive care and equitable access.
Cuba’s approach includes early detection strategies such as clinical breast exams, mammography, ultrasound, and biopsy, followed by advanced imaging and molecular diagnostics to guide treatment planning. Evidence-based therapies may involve chemotherapy, hormone therapy, radiation, and either minimally invasive or open surgical procedures, depending on the tumour’s characteristics and stage. Post-operative care, psychological support, and physical rehabilitation are also integral to recovery. With a strong foundation in clinical research and patient-centered protocols, Cuba ensures that each breast cancer treatment plan is medically rigorous, cost-effective, and personalized to achieve the best possible outcomes.
Types and Classification of Breast Cancer
Breast cancer is classified based on where it begins in the breast and its biological behavior. The main categories include:
By Location and Tissue Type
- Ductal Carcinoma in Situ (DCIS): Non-invasive cancer confined to the milk ducts.
- Invasive Ductal Carcinoma (IDC): Most common type; starts in the ducts and invades surrounding tissue.
- Invasive Lobular Carcinoma (ILC): Begins in the milk-producing lobules and spreads to adjacent tissues.
- Inflammatory Breast Cancer: A rare and aggressive form presenting with swelling and redness.
- Paget’s Disease of the Nipple: Involves the skin of the nipple and is often associated with underlying carcinoma.
By Receptor Status
- Hormone Receptor-Positive (HR+): Tumours express estrogen and/or progesterone receptors.
- HER2-Positive: Tumours overexpress the human epidermal growth factor receptor 2 protein.
- Triple-Negative Breast Cancer (TNBC): Lacks estrogen, progesterone, and HER2 receptors; more aggressive and less responsive to hormone therapy.
By Stage (TNM System)
- Stage 0–I: Early-stage, localized disease.
- Stage II–III: Regional spread to lymph nodes or nearby tissue.
- Stage IV: Metastatic breast cancer, spread to distant organs such as lungs, liver, bones, or brain.
Causes and Risk Factors of Breast Cancer
Breast cancer develops due to genetic mutations that disrupt normal cell growth. While the exact cause is often multifactorial, key risk factors include:
- Gender and age: Predominantly affects women over 50.
- Family history and genetics: Mutations in BRCA1 or BRCA2 genes increase risk.
- Hormonal exposure: Early menstruation, late menopause, or hormone replacement therapy.
- Reproductive history: Late or no pregnancies or not breastfeeding.
- Lifestyle factors: Obesity, alcohol use, physical inactivity, and high-fat diets.
- Radiation exposure: Previous chest radiation, particularly during adolescence or early adulthood.
Symptoms of Breast Cancer
Common signs and symptoms of breast cancer include:
- A new lump or thickening in the breast or underarm
- Change in breast shape or size
- Skin dimpling or puckering
- Nipple discharge (particularly if bloody or from one side only)
- Redness or scaling of the nipple or breast skin
- Inverted nipple or unusual pain
It’s important to note that not all lumps are cancerous, but all new changes should be evaluated promptly.
Diagnosis of Breast Cancer
Accurate diagnosis is essential for determining treatment options and prognosis. Diagnostic steps may include:
- Clinical Breast Exam: Performed by a physician to check for abnormalities.
- Imaging:
- Mammography: First-line screening tool.
- Ultrasound: Used for further evaluation of suspicious areas.
- MRI: For high-risk patients or ambiguous findings.
- Biopsy: Tissue sample is removed and examined under a microscope.
- Fine-needle aspiration (FNA), core needle biopsy, or surgical biopsy.
- Pathology Testing:
- Determines cancer type, grade, and receptor status (ER, PR, HER2).
- Staging Workup:
- CT scans, bone scans, or PET-CT if metastasis is suspected.
Surgical Treatment Options
Surgery remains a cornerstone in the management of breast cancer and is recommended in most cases of localized or regionally confined disease. It may also be considered in selecting metastatic cases to alleviate symptoms, reduce tumour burden, or improve local control. Surgical timing and strategy depend on tumour size, location, breast anatomy, biological subtype, patient preference, and response to systemic therapies.
Indications for surgery include:
- Localized invasive or in situ carcinoma (e.g., ductal carcinoma in situ)
- Residual tumour after neoadjuvant chemotherapy or hormone therapy
- High recurrence risk based on genetic markers or prior history
- Symptom control, such as in cases of ulceration, bleeding, or infection
- Patient preference for su
- rgical management or prophylaxis (e.g., BRCA mutation carriers)
Lumpectomy (Breast-Conserving Surgery)
Removal of the tumour and a margin of normal tissue while preserving most of the breast.
- Approach: Typically, minimally invasive, using small incisions guided by preoperative imaging or intraoperative ultrasound.
- Follow-up: Post-operative radiation therapy is usually required to reduce recurrence risk.
- Best suited for: Early-stage cancers, small tumours, or patients undergoing neoadjuvant therapy.
Mastectomy
Removal of all breast tissue, sometimes including nearby lymph nodes or skin, depending on the type.
- Types:
- Simple (Total) Mastectomy – Removes the entire breast without lymph nodes.
- Modified Radical Mastectomy – Removes the breast and axillary lymph nodes.
- Skin-Sparing Mastectomy – Preserves most of the breast skin; often paired with reconstruction.
- Nipple-Sparing Mastectomy – Preserves the nipple-areolar complex in eligible patients with peripheral tumours and no nipple involvement.
- Double Mastectomy (Bilateral Mastectomy) – Surgical removal of both breasts, performed either:
- Therapeutically in patients with bilateral breast cancer
- Prophylactically in high-risk patients (e.g., those with BRCA1 or BRCA2 mutations or strong family history), even when no cancer is present in the second breast. This approach significantly reduces the risk of developing breast cancer in the contralateral breast and is often combined with nipple- or skin-sparing techniques and immediate reconstruction for optimal cosmetic outcomes.
- Approach: Generally open surgery, though nipple-sparing mastectomies may be performed using endoscopic or robotic techniques in select centers.
- Reconstruction: May be immediate or delayed, using implants or autologous tissue (e.g., TRAM, DIEP, or latissimus dorsi flap).
Sentinel Lymph Node Biopsy
Removal of the first one or few lymph nodes (sentinel nodes) that drain lymph from the tumour.
- Technique: Minimally invasive, performed using a dye and/or radioactive tracer to identify the node.
- Benefit: If negative, patients may avoid full axillary dissection, reducing the risk of complications like lymphedema.
Axillary Lymph Node Dissection
Removal of a larger group of lymph nodes (typically levels I and II) from the axilla.
- Indicated when: Sentinel lymph node is positive for cancer or nodes are clinically suspicious preoperatively.
- Approach: Traditional open surgery, often combined with mastectomy or lumpectomy.
- Risks: Higher incidence of lymphedema, shoulder stiffness, and numbness.
Conservative (Non-Surgical) Treatment
Non-surgical treatment options can be used either as primary therapy, neoadjuvant therapy (before surgery), or adjuvant therapy (after surgery). They include:
Hormone Therapy
- Used in hormone receptor-positive cancers.
- Medications include tamoxifen, aromatase inhibitors, or ovarian suppression.
Chemotherapy
- Common in triple-negative, HER2-positive, or high-grade tumours.
- Can shrink tumours preoperatively or reduce recurrence post-surgery.
Targeted Therapy
- For HER2-positive cancers: drugs like trastuzumab, pertuzumab, or lapatinib are used to block HER2 protein.
Radiation Therapy
- Typically given after breast-conserving surgery or mastectomy (in high-risk cases).
- Destroys remaining cancer cells in the breast or lymphatic areas.
