Ataxia
Ataxia is a neurological condition that affects movement coordination and motor control, impacting various aspects of daily life. It is associated with disruptions in neural communication, which influence physical function, balance, and overall mobility. The condition can present challenges in performing routine activities, requiring individuals to develop adaptive strategies to maintain independence. Ataxia may affect different areas of life, including personal well-being, social interactions, and accessibility to support systems, highlighting the importance of comprehensive care and community awareness. Promoting understanding and support for individuals with ataxia helps create inclusive environments, enhance quality of life, and encourage further advancements in neurological research.
Why Cuba
Ataxia treatment in Cuba is carried out by a multidisciplinary team of medical professionals specializing in neurology, rehabilitation, and supportive therapies such as occupational therapy and speech therapy. The focus of treatment is on managing symptoms, improving mobility, enhancing coordination, and maintaining independence since there is no universal cure for most forms of ataxia.
By integrating medical management, physical rehabilitation, and supportive therapies, ataxia treatment in Cuba aims to help individuals adapt, improve function, and sustain independence despite the challenges posed by the condition.
Causes of Ataxia
Ataxia can develop due to several causes, both genetic and acquired. Common causes include:
- Genetic Mutations: Mutations in certain genes can cause inherited forms of ataxia. These mutations may be dominant (passed from one parent) or recessive (passed from both parents). Genetic ataxia often progresses gradually over time.
- Acquired Ataxia: This form of ataxia develops due to factors like:
- Head Trauma: Injury to the brain, especially the cerebellum.
- Stroke: Damage from lack of blood flow to parts of the brain.
- Multiple Sclerosis: A degenerative neurological disease affecting movement.
- Tumours: Growths that press on brain structures.
- Toxic Exposure: Long-term exposure to alcohol, drugs, or heavy metals like lead can damage the nervous system.
- Infections: Viral or bacterial infections such as encephalitis can cause inflammation in the brain, leading to ataxic symptoms.
Classification of Ataxia
Ataxia is typically classified based on how it is acquired and its progression rate. The main classifications include:
- Hereditary Ataxia: Passed down through genes, hereditary ataxia can be subdivided further:
- Autosomal Dominant: Faulty gene passed on from one parent.
- Autosomal Recessive: This occurs when a person inherits two copies of a faulty gene—one from each parent. If they inherit only one copy, they won’t show symptoms but will be a carrier, able to pass the gene to their children.
- Acquired Ataxia: Caused by external factors like trauma, infections, or toxins.
- Idiopathic Ataxia: In some cases, the cause remains unknown even after extensive testing. Idiopathic ataxias are typically progressive and may be diagnosed as sporadic ataxias.
Types of Ataxia
Different types of ataxias affect various bodily functions and are associated with distinct causes and symptoms:
- Cerebellar Ataxia: Occurs due to damage to the cerebellum.
- Sensory Ataxia: Results from damage to the sensory nerves in the spinal cord or peripheral nerves.
- Vestibular Ataxia: Caused by issues within the inner ear or vestibular system, responsible for balance.
- Episodic Ataxia: A rare form that occurs in episodes, triggered by stress, movement, or fatigue.
Symptoms of Ataxia
Ataxia manifests differently depending on the type and severity of the condition, but common symptoms include:
- Unsteady Gait: Difficulty walking or a staggering, unbalanced gait.
- Poor Coordination: Trouble with hand-eye coordination, often noticeable when performing tasks like writing or picking up objects.
- Slurred Speech: Speech may be slow, slurred, or appear uncoordinated (dysarthria).
- Fine Motor Skill Issues: Difficulty with small, precise movements.
- Eye Movement Abnormalities: Difficulty focusing or rapid eye movements (nystagmus).
- Tremors: Shaking or involuntary movements in hands or other body parts.
Diagnosis of Ataxia
Diagnosing ataxia involves a series of evaluations to determine the underlying cause and type. Common diagnostic methods include:
Initial Assessment:
- Gathering information about symptom onset, family history of neurological conditions, and possible exposure to toxins, medications, or infections. Questions may address the progression of symptoms, other associated neurological issues, and any recent trauma or illness.
Neurological Examination:
- A comprehensive exam assesses coordination, balance, reflexes, muscle strength, and sensory function. Tests often include gait analysis (walking patterns), finger-to-nose testing, and checking eye movements to detect abnormalities typical of specific types of ataxia (e.g., cerebellar or sensory).
- These tests collectively help isolate the area of dysfunction within the nervous system and guide further diagnostic steps to confirm the underlying cause of ataxia, providing a foundation for developing an individualized treatment plan.
Imaging Tests:
- MRI (Magnetic Resonance Imaging): Provides detailed images of the brain to detect tumours, stroke, or degeneration of cerebellar structures.
- CT Scan: A less detailed imaging method that can help rule out other causes of symptoms.
Blood Tests:
- Can help detect infections, vitamin deficiencies, or autoimmune markers that may contribute to ataxic symptoms.
Electromyography (EMG) and Nerve Conduction Studies:
- These studies are used to evaluate the health and function of muscles and peripheral nerves in patients.
- Electromyography (EMG): EMG assesses the electrical activity produced by skeletal muscles. It can reveal abnormal muscle electrical patterns, such as spontaneous muscle activity (fibrillations) or altered firing rates during contraction. For patients with ataxia, abnormal EMG findings might suggest muscle or nerve degeneration, contributing to a sensory ataxia profile.
- Nerve Conduction Studies (NCS): NCS measure the speed and strength of electrical signals traveling along nerves. This test evaluates how quickly and effectively nerves transmit signals. Delayed or diminished responses can indicate damage to the myelin sheath (the protective covering of nerves) or the nerve axon itself.
Vestibular Tests:
- Vestibular tests are essential for assessing the function of the inner ear and its role in balance and spatial orientation, particularly in cases of suspected vestibular ataxia. The vestibular system includes the inner ear structures, specifically the semicircular canals, utricle, and saccule, which detect head movements and changes in position relative to gravity. Dysfunction in this system can lead to dizziness, vertigo, unsteady gait, and coordination issues, symptoms commonly seen in vestibular ataxia.
Genetic Testing:
- Genetic testing analyzes a patient’s DNA to identify mutations associated with hereditary forms of ataxia, such as Friedreich’s ataxia or spinocerebellar ataxias. By pinpointing specific gene mutations, genetic testing provides a definitive diagnosis, clarifies inheritance patterns, and helps predict disease progression. This information is essential for tailoring treatment plans and offering family members insights into potential genetic risks.
Treatment Options for Ataxia
Currently, there is no cure for most types of ataxia, particularly hereditary forms, but various treatment approaches aim to manage symptoms, improve quality of life, and slow disease progression where possible.
In addition to symptom-specific medications and supplements, the following treatment options may be recommended:
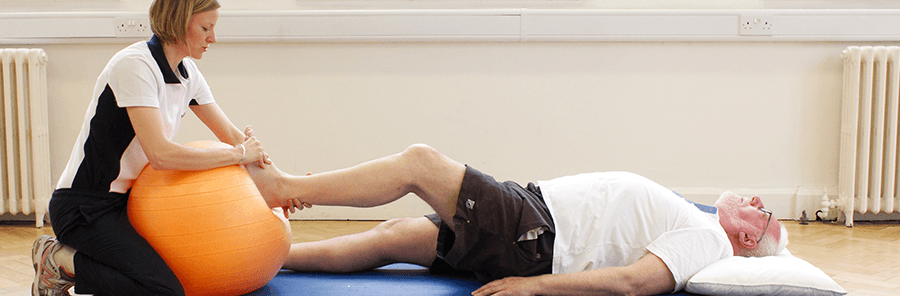
Physical Therapy:
Physical therapy is a cornerstone of managing ataxia, aimed at improving strength, coordination, balance, and overall mobility to enhance daily functioning and reduce the risk of falls. Physical therapy for ataxia is highly individualized, as patients may present with varying degrees of motor impairment and different underlying causes of the condition.
- Balance Training: These exercises are designed to challenge and improve stability, postural control and reduce fall risk.
- Strength Training: Strength exercises target major muscle groups, especially in the legs, hips, and core for maintaining stability and good posture. Improved muscle strength provides a stable foundation, aiding coordination and making daily tasks easier to perform.
- Coordination Exercises: The goal of these exercises is to improve coordination between different muscle groups.
- Gait Training: Gait training involves relearning how to walk with a more steady, predictable pattern by enhancing control over lower limb movement and stability. Gait training is essential for regaining independence in moving around safely.
- Proprioceptive Training: These are exercises that improve proprioceptive awareness (the body’s sense of its position in space) leading to better coordination and movement accuracy.
- Endurance and Stamina Building: Low-impact aerobic exercises can help build endurance without placing too much strain on the joints. Gradually increasing endurance improves a patient’s ability to handle longer periods of activity, contributing to overall mobility and quality of life.
- Home Exercise Programs: Developing home exercise programs tailored to each patient’s abilities and goals. These programs include exercises patients can practice independently or with the support of a caregiver, helping them maintain the gains achieved in therapy.
Occupational Therapy (OT):
Occupational therapy focuses on helping individuals adapt to their environment, regain functional independence, and maintain quality of life despite motor coordination challenges. Through OT, patients learn practical skills and adaptive techniques to perform daily tasks.
- Functional Task Practice: This therapy focuses on improving the ability to perform specific daily tasks that are challenging due to ataxia. By simulating real-life tasks, patients develop skills that directly translate to everyday situations, making them more independent.
- Cognitive and Sensory Training: Cognitive training exercises are carried out to maintain and enhance focus, problem-solving, and memory. Sensory training, such as differentiating textures or recognizing spatial orientation, can help improve proprioception, which may be impaired in sensory ataxia. OT also offers mindfulness techniques, helping patients adapt to changes in sensation and improving overall body awareness.
- Activities of Daily Living (ADLs) Training: ADLs include essential self-care activities like dressing, bathing, grooming, and eating. Occupational therapists break down these tasks into manageable steps, using adaptive techniques and equipment to simplify each action.
Speech Therapy:
Speech therapy plays a crucial role in the management of ataxia, particularly when the condition affects the muscles used for speech and swallowing.
- Breath Support and Control Exercises: These are exercises that strengthen respiratory muscles and improve breath control enabling individuals to produce longer, clearer sentences without running out of air. This training also contributes to voice volume, helping patients speak more audibly.
- Articulation Therapy: These are exercises that help patients improve muscle control in the tongue, lips, and jaw. Regular practice of these articulation drills improves speech clarity, allowing patients to be more easily understood.
- Swallowing Therapy (Dysphagia Management): This therapy uses swallowing exercises to strengthen the muscles involved in chewing and swallowing, improving coordination and safety.
