Cervical Cancer Treatment Program
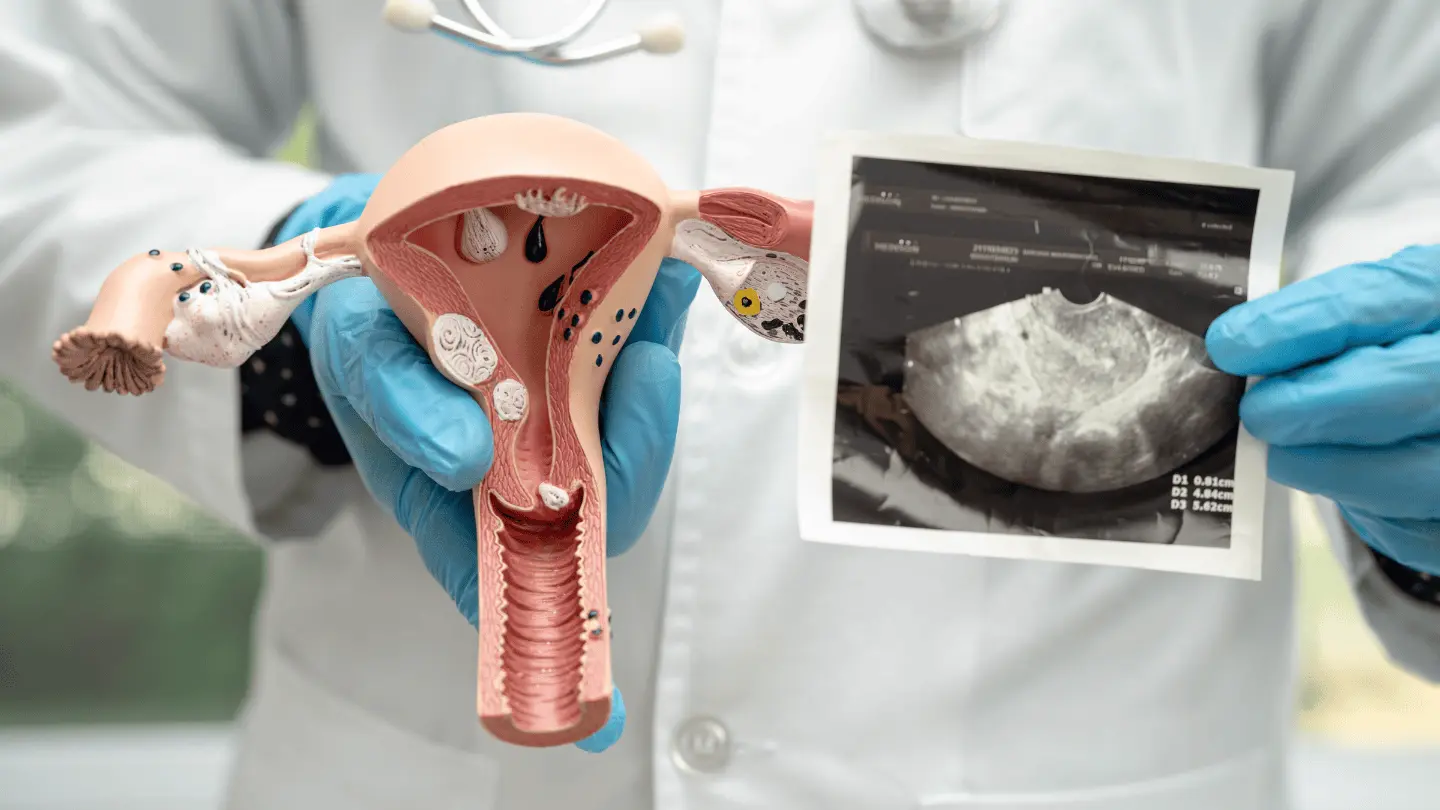
The cervix is the lower, narrow part of the uterus that connects to the vagina. It serves as the passage through which menstrual blood exits the uterus and through which a baby passes during childbirth. Cervical cancer occurs when abnormal cells in the lining of the cervix grow uncontrollably. If left untreated, these cells can invade deeper tissues of the cervix and potentially spread to other organs.
Cervical cancer is one of the most preventable and treatable forms of cancer when detected early. Routine screening and the widespread use of the HPV vaccine have significantly reduced its incidence in many parts of the world. However, it remains a leading cause of cancer-related deaths in women, particularly in low- and middle-income countries.
Why Cuba
Cervical cancer treatment in Cuba is delivered through comprehensive, multidisciplinary oncology programs specifically structured to address malignancies of the cervix at all stages. These programs are led by experienced Cuban gynecologic oncologists and supported by collaborative teams that include surgical specialists, radiologists, pathologists, and medical oncologists. Cuba’s public health system—renowned for its emphasis on prevention, early detection, and equitable access—forms the backbone of this integrated approach.
Depending on the stage and classification of cervical cancer, treatment may include chemotherapy, radiation therapy, or surgical interventions ranging from minimally invasive procedures to more extensive surgeries such as radical hysterectomy or pelvic exenteration. Cuban surgeons are proficient in both laparoscopic and open techniques, allowing them to tailor interventions to the specific characteristics of each case.
Post-treatment care in Cuba includes structured rehabilitation programs and surveillance. Cuba offers cervical cancer patients high-quality, affordable, and comprehensive care in a supportive medical environment.
Types and Classification of Cervical Cancer
Cervical cancer is primarily classified based on the type of cells in which it originates:
- Squamous Cell Carcinoma: The most common type, accounting for about 70–90% of cases. It begins in the thin, flat cells lining the outer part of the cervix.
- Adenocarcinoma: Originates in the glandular cells that produce cervical mucus. This type tends to occur higher in the cervical canal and may be more challenging to detect.
- Adenosquamous Carcinoma (or Mixed Carcinoma): A less common type that contains features of both squamous cell carcinoma and adenocarcinoma.
Causes and Risk Factors of Cervical Cancer
The primary cause of cervical cancer is persistent infection with high-risk types of Human Papillomavirus (HPV). Other contributing risk factors include:
- Early onset of sexual activity
- Multiple sexual partners
- Smoking
- Weakened immune system
- Long-term use of oral contraceptives
- Poor access to screening and healthcare
- A history of sexually transmitted infections (STIs)
Symptoms of Cervical Cancer
In its early stages, cervical cancer may not cause noticeable symptoms. As it progresses, common signs may include:
- Abnormal vaginal bleeding (e.g., after intercourse, between periods, or after menopause)
- Unusual vaginal discharge with foul odor
- Pelvic pain or pain during intercourse
- Increased urinary frequency or discomfort during urination
Because many of these symptoms can be caused by conditions other than cancer, prompt medical evaluation is essential for accurate diagnosis.
Diagnosis of Cervical Cancer
Early detection of cervical cancer relies heavily on routine screening and follow-up evaluation. Diagnostic steps may include:
- Pap Smear (Papanicolaou Test): Screens for precancerous or abnormal cells in the cervix.
- HPV Testing: Identifies high-risk HPV strains associated with cervical cancer.
- Colposcopy: A procedure using a special microscope to examine the cervix for abnormal areas.
- Biopsy: Removal of a small tissue sample from the cervix for microscopic analysis.
- Imaging Tests: MRI, CT, or PET scans may be used to determine the extent of disease spread and staging.
Cervical Cancer Treatment Options
Treatment for cervical cancer depends on the stage of the disease, the size and location of the tumour, the patient’s age and overall health, and whether fertility preservation is a priority.
Early-Stage Treatment
For Stage 0 (carcinoma in situ) and Stage I cervical cancer, the goal is complete removal of the cancerous tissue while preserving normal function as much as possible. Common options include:
- Conization (Cone biopsy):
- Conization is a diagnostic and therapeutic surgical procedure that involves removing a cone-shaped section of abnormal tissue from the cervix, including part of the endocervical canal. It is most commonly used for very early-stage cervical cancer (Stage 0 or Stage IA1) or for treating high-grade cervical dysplasia (CIN 2/3).
- Conization is typically done under local or general anesthesia and is considered minimally invasive. Most patients recover quickly, though there may be some risk of cervical stenosis or weakened cervical support in future pregnancies.
- Trachelectomy:
- A trachelectomy involves the surgical removal of the cervix, the upper portion of the vagina, and surrounding parametrial tissue, while preserving the uterus. This fertility-sparing procedure is typically recommended for young women with early-stage cervical cancer (Stages IA2 to IB1) who wish to retain the ability to become pregnant.
- There are two main approaches:
- Vaginal radical trachelectomy (performed through the vaginal canal, often with laparoscopic lymph node assessment)
- Abdominal radical trachelectomy (open or laparoscopic abdominal approach)
- In both cases, the pelvic lymph nodes are usually removed to check for cancer spread. Permanent cerclage (a stitch to support the uterus) is typically placed at the uterine opening to support future pregnancies. Recovery is generally faster than traditional hysterectomy, and many women go on to conceive, although they are considered high-risk pregnancies.
- Simple or Radical Hysterectomy:
- A hysterectomy is the surgical removal of the uterus and cervix, and it may be classified as simple or radical, depending on how much surrounding tissue is also removed.
- Simple Hysterectomy involves removal of just the uterus and cervix. It is generally used for very early-stage cervical cancer or for certain pre-cancerous conditions.
- Radical Hysterectomy involves removal of the uterus, cervix, upper vagina, and parametrial tissues (the connective tissue around the cervix), and often includes pelvic lymph node dissection. This procedure is used for Stage IB to IIA cervical cancers.
- Hysterectomies can be performed using different techniques:
- Open abdominal surgery (traditional)
- Laparoscopic surgery (minimally invasive)
- Recovery time and postoperative complications vary depending on the surgical method and the extent of the procedure.
- Patients undergoing a radical hysterectomy will no longer be able to conceive and may require hormone management if the ovaries are removed as well.
Locally Advanced Disease
In Stage II to Stage III cervical cancer, the tumour has spread beyond the cervix into nearby tissues such as the upper vagina, parametrium, or pelvic walls, but has not reached distant organs like the lungs, liver, or bones. At this stage, the disease is considered locally advanced, and the primary goal of treatment is to control the tumour locally, prevent further spread, and preserve organ function where possible.
In most cases, surgery is not recommended as a primary treatment since the tumour has spread to areas that make complete surgical removal difficult or impossible without causing significant damage. However, in selected patients, surgery might be done to relieve symptoms (e.g., severe bleeding or obstruction), but not as a curative approach.
- Radiation Therapy
- Radiation therapy plays a central role in the treatment of locally advanced cervical cancer. It uses high-energy X-rays or particles to destroy cancer cells and shrink tumours.
- Radiation therapy is carefully planned using advanced imaging (CT, MRI, or PET scans) to ensure precise targeting, reduce side effects, and protect the bladder, rectum, and intestines from excessive radiation exposure.
- Chemoradiation
- Chemoradiation refers to the concurrent use of chemotherapy and radiation therapy. In this combined approach:
- Chemotherapy is administered at low doses—typically once a week—during the course of external radiation therapy.
- Its primary function is to act as a radiosensitizer, making cancer cells more vulnerable to the effects of radiation.
- Chemoradiation refers to the concurrent use of chemotherapy and radiation therapy. In this combined approach:
While chemoradiation is highly effective, it can also lead to cumulative side effects such as fatigue, gastrointestinal discomfort, skin irritation in the treated area, changes in bowel or bladder habits, and temporary or permanent reproductive changes. These effects are carefully managed by the oncology care team to maintain the patient’s quality of life during and after treatment.
Advanced or Metastatic Disease
- When cervical cancer has spread to distant organs such as the lungs, liver, or bones—a condition known as metastatic or Stage IVB disease—the treatment approach shifts from curative to palliative.
- The focus is no longer on eliminating the disease entirely but rather on slowing its progression, alleviating symptoms, and enhancing the patient’s overall quality of life.
- The goal is to help the patient maintain the highest possible level of physical and emotional well-being, often through a coordinated, multidisciplinary care plan that includes ongoing medical support, psychological counseling, and, when appropriate, end-of-life planning.
Post-Treatment Surveillance
After treatment, regular follow-ups are essential to monitor for recurrence and manage any long-term side effects. This includes:
- Pelvic exams
- Imaging (ultrasound, MRI, or CT scans)
- HPV testing and Pap smears (when applicable)
Supportive and Rehabilitative Care
Cervical cancer treatment can impact physical, emotional, and reproductive health. Rehabilitation services, psychological support, and fertility counseling are often part of comprehensive care.
