Ovarian Cancer Treatment Program
The ovaries are a pair of small, almond-shaped organs located on either side of the uterus in the female reproductive system. Their primary roles include the production of eggs (ova) for fertilization and the secretion of essential reproductive hormones, including estrogen and progesterone. These hormones regulate the menstrual cycle, influence fertility, and impact other aspects of a woman’s overall health, including bone density and cardiovascular function.
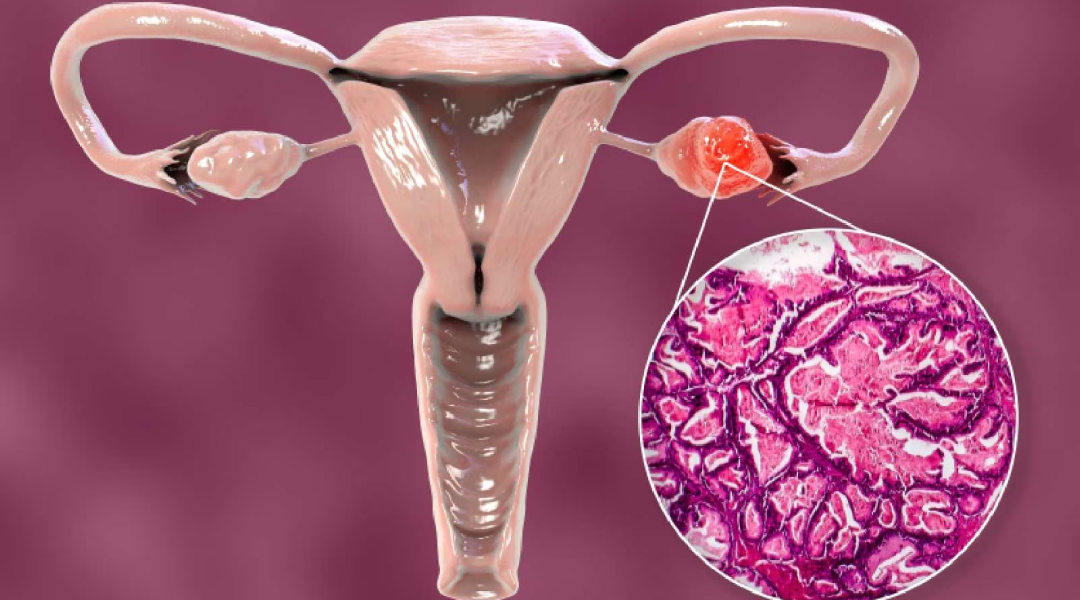
Ovarian cancer occurs when cells within the ovary undergo genetic mutations that cause them to grow uncontrollably and evade normal regulatory mechanisms. These abnormal cells eventually form a malignant tumour, which can invade surrounding tissues and, if left untreated, spread to other parts of the body through the lymphatic system, bloodstream, or direct extension into the abdominal cavity.
This disease is considered one of the most serious and life-threatening gynecologic malignancies primarily because it is often diagnosed at an advanced stage. In its early phases, ovarian cancer usually does not produce specific or noticeable symptoms, and when symptoms do appear, they tend to be subtle, vague, or easily attributed to common gastrointestinal or urinary issues, such as bloating, mild pelvic discomfort, or changes in bowel habits. As a result, many cases go undetected until the cancer has progressed significantly, reducing the chances of successful treatment and long-term survival.
Why Cuba
Ovarian cancer treatment in Cuba is delivered through comprehensive, multidisciplinary oncology programs designed to manage malignancies of the ovaries across all stages. These programs are led by experienced Cuban gynecologic oncologists and supported by a coordinated network of specialists, including surgical oncologists, radiologists, pathologists, and medical oncologists.
Treatment strategies in Cuba are determined based on the type, grade, and stage of ovarian cancer, as well as the patient’s overall health and treatment goals. Therapeutic options may include surgery and systemic chemotherapy. Surgical interventions range from traditional open procedures to minimally invasive techniques such as laparoscopy, depending on tumour size, disease spread, and individual clinical factors. The primary goal is to remove as much of the tumour as possible while minimizing surgical complications and promoting optimal recovery.
Cuban oncology centers emphasize personalized treatment planning in accordance with internationally recognized clinical guidelines. Following active treatment, patients benefit from structured follow-up protocols that include rehabilitation support, ongoing medical evaluation, and long-term surveillance to detect recurrence and manage late effects of treatment.
Types and Classification of Ovarian Cancer
Ovarian cancer is not a single disease but a group of malignancies that arise from different types of cells within the ovary. The three main classifications include:
- Epithelial Ovarian Cancer (90% of cases)
- Arises from the outer surface lining of the ovary.
- Subtypes include serous, mucinous, endometrioid, and clear cell carcinomas.
- High-grade serous carcinoma is the most aggressive and common subtype.
- Germ Cell Tumours
- Originate from the cells that form eggs.
- Typically occur in younger women and are often highly treatable.
- Stromal (Sex Cord-Stromal) Tumours
- Develop from the connective tissue cells that produce hormones.
- May secrete estrogen or androgens, sometimes causing hormonal symptoms.
Causes and Risk Factors of Ovarian Cancer
While the precise cause of ovarian cancer remains unknown, several risk factors have been identified:
- Age: Most cases occur in women over 50, with the highest incidence after menopause.
- Family History: Having close relatives with ovarian, breast, or colorectal cancer increases risk.
- Genetic Mutations: Inherited mutations in genes such as BRCA1, BRCA2, or those associated with Lynch syndrome significantly raise the risk.
- Reproductive History: Women who have never been pregnant or who experienced infertility have a slightly higher risk.
- Hormonal Factors: Long-term use of hormone replacement therapy (HRT) may increase risk.
- Endometriosis: A condition where tissue similar to the uterine lining grows outside the uterus, potentially increasing the risk for certain ovarian cancer subtypes.
Symptoms of Ovarian Cancer
Ovarian cancer is often called the “silent killer” because its early symptoms can be subtle and non-specific. However, common signs include:
- Persistent bloating or abdominal swelling
- Pelvic or abdominal pain
- Difficulty eating or feeling full quickly
- Frequent or urgent urination
- Fatigue
- Back pain
- Unexplained weight loss
- Changes in bowel habits (e.g., constipation)
Any symptoms that persist for more than a few weeks should prompt medical evaluation, especially in postmenopausal women.
Diagnosis of Ovarian Cancer
A diagnosis of ovarian cancer typically involves a combination of clinical evaluation, imaging, and laboratory testing:
- Pelvic Examination: May detect masses or abnormalities in the ovaries or surrounding tissues.
- Transvaginal Ultrasound (TVUS): Provides detailed imaging of ovarian structure.
- CA-125 Blood Test: Measures a protein that may be elevated in ovarian cancer, although it is not specific and can be elevated in benign conditions.
- CT Scan or MRI: Used to assess the extent of disease and guide surgical planning.
- Biopsy or Surgical Exploration: Often performed during surgery to confirm diagnosis and perform staging.
Definitive diagnosis usually requires surgical removal of the tumour, followed by pathological analysis.
Types of Treatment for Ovarian Cancer
Treatment for ovarian cancer depends on the stage, grade, and type of tumour, as well as the patient’s age, general health, and treatment goals.
Surgery
- Surgery is the cornerstone of treatment for ovarian cancer, especially in newly diagnosed cases. It plays a dual role—both diagnostic and therapeutic—by confirming the extent of disease and removing as much cancerous tissue as possible. The goal is to achieve optimal cytoreduction, which significantly improves the effectiveness of subsequent treatments such as chemotherapy and is closely linked to improved survival outcomes.
- Cytoreductive (Debulking) Surgery
Cytoreductive, or debulking, surgery aims to remove all visible tumour tissue, or as much as is safely possible. It is considered the primary and most critical intervention in the treatment of advanced ovarian cancer. The success of this procedure—defined as leaving no residual disease or tumour deposits less than 1 cm in size—directly correlates with better prognosis and response to chemotherapy.
- Cytoreductive (Debulking) Surgery
- This comprehensive surgical procedure often includes:
- Total hysterectomy (removal of the uterus)
- Bilateral salpingo-oophorectomy (removal of both ovaries and fallopian tubes)
- Omentectomy (removal of the omentum, a fatty layer where ovarian cancer frequently spreads)
- Pelvic and para-aortic lymph node dissection (to assess and remove cancer-involved lymph nodes)
- In some cases, resection of parts of the bowel, diaphragm, liver surface, or peritoneum if tumour spread is extensive
- This comprehensive surgical procedure often includes:
- Surgery for ovarian cancer can be performed:
- Open Surgery (Laparotomy): This is the most common approach, especially in cases of widespread disease. It provides full access to the abdominal cavity, allowing the surgeon to thoroughly inspect and remove tumour tissue from multiple sites.
- Minimally Invasive Surgery (Laparoscopy or Robotic-Assisted): This may be considered for early-stage disease in carefully selected patients. It involves smaller incisions, less postoperative pain, shorter hospital stays, and faster recovery. However, it is not generally recommended for advanced cases due to the need for extensive tissue removal.
Chemotherapy
- Chemotherapy is a critical component of ovarian cancer treatment. It plays a central role in managing both early-stage high-risk cancers and widespread disease, improving overall survival and reducing the risk of recurrence.
- Adjuvant Chemotherapy: Most commonly given after cytoreductive surgery, adjuvant chemotherapy targets microscopic residual cancer cells that may not have been removed during surgery. This reduces the likelihood of recurrence and is considered standard for all but the earliest-stage, low-grade tumours.
- Neoadjuvant Chemotherapy: In some cases, particularly when the disease is extensive or the patient is not initially fit for major surgery, chemotherapy is given before surgery to shrink tumours. This approach helps make surgery safer and more effective. It is typically followed by interval debulking surgery and additional chemotherapy cycles.
Hormonal Therapy
- While not a frontline treatment for most ovarian cancers, hormonal therapy can play a valuable role in managing select cases, particularly in patients with low-grade, slow-growing, or recurrent tumours that are known to be responsive to hormonal regulation. This approach is most often used when traditional treatments such as surgery or chemotherapy are not appropriate or have already been exhausted.
- Hormonal therapy is generally considered for:
- Low-grade serous carcinomas of the ovary, which tend to grow more slowly and may be influenced by hormonal activity.
- Recurrent ovarian cancer, especially in women who prefer less intensive treatment or who are not candidates for additional chemotherapy.
- Palliative care in advanced disease, to slow progression while maintaining quality of life.
Radiation Therapy
- Although not a primary treatment for most ovarian cancers, radiation therapy can serve an important role in specific clinical situations, particularly in cases of localized recurrence, persistent disease, or for palliative symptom relief. It involves the use of high-energy radiation to destroy cancer cells or shrink tumours in targeted areas.
- Radiation therapy may be considered for:
- Isolated recurrences in the pelvis or abdominal wall, especially when surgery or chemotherapy is not feasible.
- Palliative care, to relieve symptoms such as pain, bleeding, or pressure caused by tumour growth in advanced disease.
- Residual disease, when small, localized cancer deposits remain after primary treatment.
