Endometrial (Uterine) Cancer Treatment Program
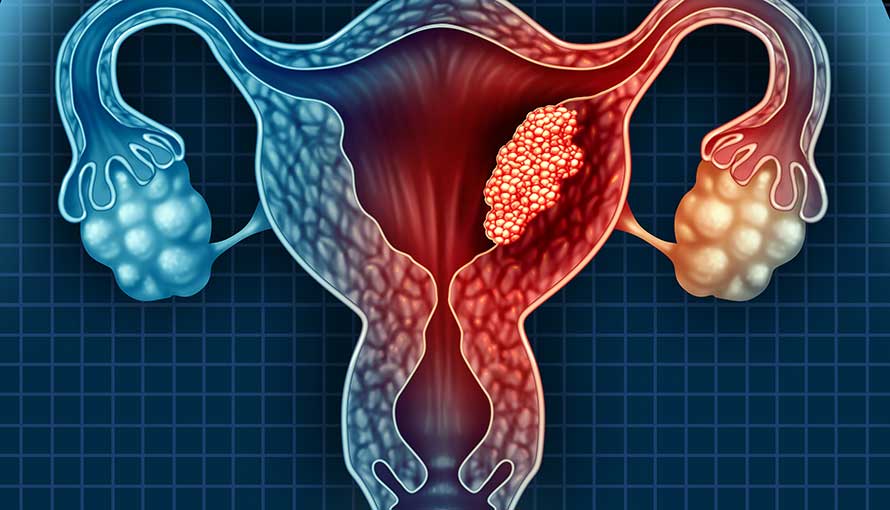
The uterus is a hollow, pear-shaped organ located in the female pelvis, responsible for housing and nurturing a developing fetus during pregnancy. It is composed of different layers, with the endometrium forming the inner lining that thickens and sheds with each menstrual cycle.
Endometrial cancer, also referred to as uterine cancer, specifically originates in the endometrial lining. It is the most common type of cancer affecting the uterus. Although “uterine cancer” can refer to malignancies arising from any part of the uterus, the vast majority originate from the endometrium, hence the interchangeable use of the terms. Rarely, cancer may develop in the muscular layer of the uterus, known as uterine sarcoma.
Early detection of endometrial cancer is often possible due to noticeable symptoms such as abnormal uterine bleeding, making it one of the more treatable gynecologic cancers when diagnosed in the early stages.
Why Cuba
Endometrial (uterine) cancer treatment in Cuba is managed through integrated, multidisciplinary oncology programs designed to address malignancies of the uterine lining across all stages. These programs are led by highly trained Cuban gynecologic oncologists and supported by collaborative teams that include surgical oncologists, radiologists, pathologists, and medical oncologists.
Depending on the type, grade, and stage of endometrial cancer, treatment options in Cuba may include surgical intervention, radiation therapy, hormonal therapy, and systemic chemotherapy. Surgical procedures may be traditional open or minimally invasive techniques depending on the patient’s clinical profile and are aimed at achieving complete tumour removal while minimizing recovery time and complications.
Cuban cancer centers emphasize personalized treatment planning that adheres to internationally accepted protocols. Post-treatment care includes structured rehabilitation services, hormonal support when indicated, and long-term surveillance to monitor for recurrence. Cuba offers patients with endometrial cancer a high standard of care in a medically advanced and supportive environment.
Types and Classification of Endometrial (Uterine) Cancer
Endometrial cancers are classified based on their cellular origin and behaviour:
- Endometrioid Adenocarcinoma: The most common form, arising from the glandular cells of the endometrium. It typically has a favorable prognosis when caught early.
- Serous Carcinoma: A more aggressive, non-endometrioid type that tends to spread rapidly and has a poorer prognosis.
- Clear Cell Carcinoma: Another rare and aggressive variant, often diagnosed at a more advanced stage.
- Uterine Carcinosarcoma (Malignant Mixed Müllerian Tumour): Contains both carcinomatous and sarcomatous components and behaves more aggressively.
- Uterine Sarcomas: These include leiomyosarcomas and endometrial stromal sarcomas, which arise from the muscle or connective tissue of the uterus rather than the endometrial lining.
Causes and Risk Factors of Endometrial (Uterine) Cancer
The exact cause of endometrial cancer is not always known, but several risk factors have been identified:
- Hormonal Imbalance: Prolonged exposure to estrogen unopposed by progesterone (e.g., due to obesity, hormone therapy, polycystic ovary syndrome, or estrogen-secreting tumours).
- Obesity: Excess fat tissue increases estrogen levels, raising the risk.
- Age: Most cases occur in women over the age of 50.
- Family History and Genetics: A family history of endometrial or colorectal cancer may increase risk, particularly in those with Lynch syndrome (hereditary nonpolyposis colorectal cancer).
- Menstrual and Reproductive History: Early menstruation, late menopause, infertility, or not having children are associated with increased risk.
- Diabetes and Hypertension: These chronic conditions are commonly seen in patients with endometrial cancer.
Symptoms of Endometrial (Uterine) Cancer
One of the advantages of endometrial cancer is that it often presents early with symptoms, allowing for earlier diagnosis. Common signs include:
- Abnormal Uterine Bleeding: Especially postmenopausal bleeding, or irregular bleeding in premenopausal women.
- Pelvic Pain or Cramping
- Pain During Intercourse
- Unusual Vaginal Discharge: Especially if watery, pink, or blood-tinged.
- Unexplained Weight Loss or Fatigue (in more advanced stages)
Any abnormal bleeding, particularly after menopause, should prompt immediate medical evaluation.
Diagnosis of Endometrial (Uterine) Cancer
Diagnosing endometrial cancer involves a combination of clinical evaluation and diagnostic procedures:
- Pelvic Examination: A physical exam to check for abnormalities in the uterus or surrounding structures.
- Transvaginal Ultrasound: Provides imaging of the endometrial thickness and structure.
- Endometrial Biopsy: A sample of the endometrial tissue is taken and examined for cancer cells.
- Hysteroscopy: Allows direct visualization of the uterine cavity using a thin, lighted tube.
- Dilation and Curettage (D&C): A more extensive sampling procedure if biopsy results are inconclusive.
- Imaging Tests (CT, MRI, PET): To assess the spread of disease and aid in staging.
Endometrial (Uterine) Cancer Treatment Options
Treatment for endometrial (uterine) cancer is based on the type, stage, and grade of the disease and typically involves a combination of surgery, radiation, hormonal therapy, and in some cases, chemotherapy—each tailored to the individual patient’s clinical profile and overall health.
Surgery
- Surgery is the cornerstone of treatment for most cases of endometrial cancer, especially when the disease is diagnosed at an early stage. The surgical approach aims to remove the primary tumour, assess the extent of spread, and determine the need for any additional therapies. The extent and type of surgery depends on the stage, tumour grade, histologic subtype, patient’s age, general health, and fertility considerations.
- Hysterectomy
A hysterectomy is the primary surgical procedure for endometrial cancer and involves the removal of the uterus. In the vast majority of cases, this procedure is extended to include the fallopian tubes and ovaries—a procedure known as a total hysterectomy with bilateral salpingo-oophorectomy (BSO). Removing the ovaries reduces the hormonal stimulation that may contribute to cancer progression and eliminates potential sites for metastasis.
- Hysterectomy
- Depending on the patient’s condition and disease extent, the hysterectomy may be performed through:
- Abdominal incision (open surgery)
- Vaginal approach
- Minimally invasive techniques such as laparoscopy or robotic-assisted laparoscopy
- Depending on the patient’s condition and disease extent, the hysterectomy may be performed through:
- Lymphadenectomy
In cases where there is a risk of lymphatic spread, surgeons may perform a lymphadenectomy, which involves the removal of pelvic and para-aortic lymph nodes. These lymph nodes are examined under a microscope to determine whether cancer has spread beyond the uterus.
- Lymphadenectomy
- Lymph node assessment helps refine staging and guide decisions on post-surgical therapies such as chemotherapy or radiation. In select early-stage, low-risk cases, lymphadenectomy may be omitted or replaced with sentinel lymph node mapping, a technique that identifies and removes only the first nodes most likely to contain cancer.
- Minimally Invasive Surgical Techniques
For women diagnosed with early-stage endometrial (uterine) cancer, minimally invasive surgery has become the preferred approach due to its proven safety, effectiveness, and improved recovery profile compared to traditional open surgery. These techniques offer the same oncologic outcomes as open procedures but with fewer complications and a better overall surgical experience, especially for patients with other health conditions such as obesity or diabetes.
- Minimally Invasive Surgical Techniques
- Not all patients with uterine (endometrial) cancer are ideal candidates for minimally invasive surgery. Patients who may not qualify typically include those with the following conditions:
- Advanced-stage cancer
- Extensive adhesions or scar tissue
- Morbid obesity (in certain cases)
- Very large uterus or tumour bulk
- Poor cardiopulmonary status
- Suspected lymph node or omental involvement
Radiation Therapy:
- Radiation therapy is a key component of treatment for endometrial cancer, particularly in patients with high-risk features, more advanced disease, or those who are not candidates for surgery. It uses high-energy beams to destroy cancer cells and reduce the likelihood of recurrence by targeting areas where cancer might remain after surgical removal—or, in some cases, as a primary treatment when surgery is contraindicated.
- For women who are medically unfit for surgery—due to age, frailty, or significant comorbidities—radiation therapy can used as a primary treatment.
Hormonal Therapy:
- Hormonal therapy plays an important role in the treatment of select cases of endometrial cancer, especially when preserving fertility is a priority or when surgery is not recommended due to medical or personal reasons. This approach targets the hormone-sensitive nature of many endometrial cancers by modifying the body’s hormonal environment to slow or stop tumour growth.
- Early-stage, low-grade cancers: Particularly in younger women who wish to retain the ability to become pregnant, hormonal therapy may be used as a conservative treatment alternative to hysterectomy.
- Patients unfit for surgery: In women with significant comorbidities or frailty, hormonal therapy may serve as a primary treatment to control disease progression when surgery or radiation is not appropriate.
- Recurrent or residual disease: Hormonal therapy may be used to manage slow-growing tumours that reappear after initial treatment, especially when the recurrence is limited and not aggressive.
Chemotherapy:
- Chemotherapy is a key treatment modality for endometrial cancer, particularly in advanced stages, high-grade tumours, or when the cancer has spread beyond the uterus. Unlike localized treatments such as surgery or radiation, chemotherapy is a systemic therapy—it circulates throughout the body via the bloodstream, making it effective for targeting cancer cells that may have spread to distant organs or lymph nodes.
- Advanced-Stage Disease (Stage III or IV): When cancer has extended into the pelvic structures, abdominal cavity, or distant sites.
- High-Grade Histology: Tumours such as serous carcinoma, clear cell carcinoma, or carcinosarcoma, which tend to grow and spread more aggressively.
- Recurrent Disease: When cancer returns after initial treatment, chemotherapy may help control its progression.
- Adjuvant Setting: Given after surgery to reduce the risk of recurrence in patients with poor prognostic factors.
- Neoadjuvant Setting: Occasionally used before surgery to shrink large tumours and improve surgical outcomes.
